Mohs Surgery NYC: Minimally Invasive Skin Cancer Treatment
A precise, outpatient surgical procedure for skin cancer
- Last Updated: April 24, 2025
- By Julia Tzu, MD FAAD
If you’ve been diagnosed with skin cancer like basal cell carcinoma or squamous cell carcinoma, it’s natural to feel anxious—especially when it affects cosmetically sensitive areas like the face. You want the cancer removed completely, but you also want to minimize scarring and preserve your appearance.
At Wall Street Dermatology, our Mohs surgery in NYC is performed by Dr. Julia Tzu, a triple board-certified dermatologist who is both fellowship-trained in Mohs surgery and board-certified in dermatopathology. With her background from Stanford, Johns Hopkins, the University of Miami, NYU, and the University of Pennsylvania, Dr. Tzu offers an unparalleled combination of diagnostic precision and surgical expertise. Patients across New York City are referred to us for outstanding outcomes in both skin cancer removal and cosmetic reconstruction.
If you’ve been diagnosed with skin cancer, don’t leave your treatment or appearance to chance—schedule your consultation with Dr. Julia Tzu at Wall Street Dermatology for Mohs surgery in NYC.
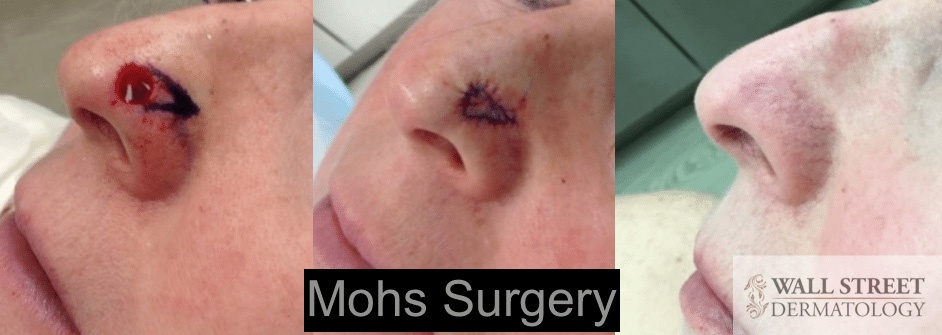
Mohs Surgery Outcomes
Skin cancer surgery on the face can cause much anxiety for patients because the face is an exquisitely cosmetically-sensitive area. A trained Mohs surgeon can generate excellent aesthetic outcomes on facial areas such as your nose, forehead, eyelids,and cheeks.
Below is a surgery involving the nose, and the post-surgery outcome after approximately 6 months.
Below is a surgery involving the forehead and cheek, and the post-surgery outcome also after approximately 6 months.
Dermatologist Dr. Julia Tzu’s Perspective on Mohs Surgery
“People are often frightened by the idea of skin cancer surgery, because images of big, unsightly scars come to mind. However, my patients are usually pleasantly surprised by the inconspicuous nature of their post surgical scars due to my precise surgical technique combined by the minimally invasive nature of Mohs surgery.” – Dr. Julia Tzu, MD, FAAD
Mohs Surgery Process: What You Can Expect?
Mohs surgery is a sophisticated outpatient procedure that removes skin cancer in stages by excising small layers of skin one step at a time and visualizing the excised skin under the microscope until the skin cancer is completely removed.
Performed by triple board-certified dermatologists like Dr. Julia Tzu, who has undergone official American College of Mohs Surgery (ACMS) fellowship training as well as board certification in Mohs micrographic surgery, this approach is precise, effective, and tissue-conserving. It boasts the highest cure rate among conventional skin cancer treatments.
Mohs micrographic surgery should be performed by qualified dermatologic surgeons who are expertly fellowship-trained and board certified in the three components of the procedure, which are detailed below.
How to Prepare for Mohs Surgery
To help ensure a safe and smooth procedure, you’ll need to stop taking certain medically unnecessary medications and supplements that can increase bleeding about 10-14 days before surgery. These include ibuprofen, naproxen, aspirin (unless medically necessary), fish oil, vitamin E, and herbal supplements like ginkgo biloba and ginseng. If you’re on prescription blood thinners, speak with your prescribing doctor to see if temporary adjustments are possible. Avoid alcohol for at least 48 hours before surgery, and try to stop smoking for at least a week beforehand to promote better healing.
On the day of surgery, bring something interesting to read or watch to pass the time, eat a light meal, wear comfortable clothing that’s easy to remove without pulling over your head, and plan to spend half to an entire day at the office as the procedure is done in stages. Most patients do well with local anesthesia and can drive themselves, but arranging a ride is a good idea if your surgery is near the eyes or if you’re feeling anxious. Be sure to inform our Mohs surgeon of any allergies or medical conditions prior to the procedure.
Skin Cancer Tissue Removal
Before the procedure begins, we use a local injection of anesthesia to numb the area and ensure that you’re comfortable during the surgery. Our Mohs surgeon will then excise the visible tumor and a very thin layer of the surrounding skin.
A technician will then use the excised tissue sample to prepare microscope slides for the surgeon to examine. If our Mohs surgeon sees cancerous cells around the sample’s edges, they’ll remove another thin layer of tissue from only the area that harbors the skin cancer cells. Your surgeon will continue to examine the excised tissue and remove layers until they reach a layer of healthy tissue that is cancer-free with clean margins.
This process is usually performed in stages, usually ranging between one to three stages. More complicated skin cancers can involve more than three stages. Since the Mohs surgeon removes only a small amount of tissue at a time, more skin is preserved, minimizing distortion of important facial structures as well as scarring.
Lab Analysis
Wall Street Dermatology also has an on-site Mohs laboratory to prepare slides for the Mohs surgeon to interpret and analyze in real time. From a medical standpoint, this is the most critical part of Mohs micrographic surgery.
Dr. Julia Tzu is one of few Mohs surgeons who is not only board certified in Mohs surgery, but also board certified in dermatopathology (the discipline of reading skin tissue samples). While board certification in dermatopathology is not necessary to practice Mohs surgeon, it confers an extra degree of expertise in interpretation of more complex skin cancer tissue samples.
Your Mohs surgeon must carefully analyze each excised tissue sample under a microscope to determine whether the surgery is complete. Their goal is to remove as little tissue as possible while completely eradicating all cancerous cells from the area.
Reconstruction
Once the tumor and all cancerous cells have been removed, your Mohs surgeon will close and, if necessary, reconstruct the surgical wound to minimize the appearance of scarring and preserve your facial shape.
Before your Mohs micrographic surgery, we’ll conduct a consultation with you to determine how much reconstruction may be necessary, depending on the size and shape of the tumor. Your Mohs surgeon will use information from this consultation and their findings during the surgery to determine which reconstruction technique is best.
Common post-Mohs surgery reconstruction techniques include:
- Self-healing for smaller, more superficial surgical wounds
- Side-to-side sutured closure for larger wounds
- Skin grafts to close larger or more complex wounds not amenable to other forms of closure.
- Skin flaps to close larger or more complex wounds not amenable to other forms of closure.
- Referral to a facial reconstruction specialist, if needed
Mohs Surgery Cancer Prognosis
Mohs surgery has a 93-97% success rate when it comes to eradicating skin cancer. Excising and examining one layer of tissue at a time ensures complete cancer removal and dramatically decreases the chances of the skin cancer coming back.
Patients that opt for Mohs surgery also typically have a better psychological outcome because the procedure preserves their appearance as much as possible. Combined with the peace of mind from being cancer-free, Mohs surgery patients endure less stress than those undergoing other techniques.
Recovery After Mohs Surgery
Recovery after Mohs surgery is usually quick and straightforward. You may have mild swelling, bruising, or discomfort for a few days, which can be managed with Tylenol. Your doctor will give you clear instructions on how to care for the wound, change bandages, and apply ointment to help with healing and reduce scarring. Most patients can return to normal activities within a few days, but you should avoid strenuous exercise and heavy lifting for at least 48 hours. If you notice increased redness, pain, or drainage, contact Dr. Tzu right away.
How Does a Dermatologist Diagnose Skin Cancer?
Before Mohs surgery is considered as a treatment option, the first step is for a dermatologist specializing in skin cancers to diagnosis suspicious growths on the skin. While skin cancer can, in many instances, be visually diagnosed by an experienced dermatologist, a skin biopsy is the gold standard for diagnosing skin cancer and is necessary before any specific treatment can be recommended. During a skin biopsy, the skin is anesthetized by a quick injection, and a small sliver of skin is removed from the suspected skin cancer, and then sent to a laboratory for a dermatopathologist (read more on what is a dermatopathologist) to analyze under the microscope and interpret. A pathology report that contains the diagnosis is then generated based on the dermatopathologist’s findings
Choosing a Mohs Surgeon in NYC
Fortunately, New York City has some of the leading dermatologists and skin surgery centers specializing in Mohs micrographic surgery.
Factors you should consider include:
- Facility Type: Surgeries can be performed at University Hospitals like NYU (where Dr. Tzu is a part-time assistant professor). From a cost perspective, extra facility fees apply to hospital-based surgery. Surgeries can also be performed at outpatient office facilities such as Wall Street Dermatology. From a cost perspective, no facility fees apply to office-based surgery.
- Availability: Don’t delay treating skin cancer. Schedule your appointment for skin cancer surgery sooner than later.
- Credentials and Experience of the Mohs Surgeon: Dr. Tzu is fellowship-trained in dermatopathology (NYU 2010) and Mohs and reconstructive surgery (University of Pennsylvania 2011). The majority of Mohs surgeons are not board certified in dermatopathology.
- Time Allocated to Procedure: Will your dermatologist spend the extra time to ensure your skin cancer is completely removed and your cosmetic outcomes are as optimal as possible? Some medical practices performing Mohs surgeries cycle 10-20 cases per day per Mohs surgeon. At Wall Street Dermatology, we intentionally cap our Mohs surgery cases to 5 per day to give ample time for both the Mohs surgery and the reconstruction, which we believe leads to better outcomes.
How Much Does Mohs Surgery Cost in NYC?
For self pay, Mohs surgery in NYC typically costs between $3000 to $4000, although it could be higher depending on the extent of your surgery. Since Mohs surgery is considered medically necessary, it’s usually covered by insurance. However, coverage varies based on what kind of health insurance you have, and one’s out of pocket financial responsibility depends on whether there is an unmet deductible.
Where Is Mohs Surgery Performed with Wall Street Dermatology?
Mohs surgery at Wall Street Dermatology is performed on an outpatient basis in our Financial District medical practice, which is equipped with a specialized Mohs laboratory. In addition to our existing staff, we have a highly experienced Mohs technician that assists with laboratory tissue preparation. Performed under local anesthesia, confirmed skin cancer removal is achieved within a day, and patients remain monitored in patient rooms until it is safe for them to be discharged from the office.
Dr. Julia Tzu’s Expertise as a Mohs Surgeon
Dr. Julia Tzu is double board certified, and dual fellowship trained in both dermatopathology, the study of skin tissue analysis, as well as Mohs micrographic surgery and skin reconstruction.
Her dermatopathology fellowship training was completed at New York University Hospital, a referral center for some of the most complex skin tumor diagnostic cases. This means that Dr. Tzu has the specialized training to interpret skin cancer slides with a level of expertise beyond most Mohs surgeons. Dermatopathology board certification is not required for Mohs surgeons, but is advantageous in instances where more difficult tumor recognition and diagnoses are needed.
Dr. Tzu’s fellowship training in Mohs and reconstructive surgery was completed at the Hospital of the University of Pennsylvania, a referral center for the most complex Mohs surgical cases in the Northeast. Her experience with complex surgical reconstruction allows her to perform the majority of her reconstructions in-house, without the need to refer to an outside hospital or surgical center. She is well-known for her focus on scar cosmesis and aesthetic outcomes. She is a member of the exclusive American College of Mohs Surgery, membership of which is only granted to fellowship trained, board certified dermatologists who have completed all the formal academic, institutional, and experiential requirements to meet rigorously defined standards.
Dr. Tzu is a clinical assistant professor and attending at NYU Hospital, where she teaches surgery to dermatology resident physicians on a weekly basis.
Get Mohs Surgery From a Triple Board-Certified Dermatologist
Below are some Q&A that we have frequently received from Mohs surgery patients. If you have questions following a Mohs surgery diagnosis, or if you believe you are at risk of a skin cancer that may require it, we invite you to schedule an appointment at Wall Street Dermatology, and let Dr. Julia Tzu guide you through the next steps.
Mohs Surgery FAQ
Is Mohs surgery only done on the face?
Mohs surgery may be performed on several areas of the body to treat basal cell, squamous cell carcinomas, and other types of skin cancers. Areas where Mohs surgery may be the best choice include:
- Near the eyes
- Nose or lips
- Ears or scalp
- Genitals
- Neck
- Hands and Feet
- Anywhere on the face
Can the Mohs surgery wound heal without stitches?
If the surgical wound is small enough, Mohs surgery can heal without stitches. However, most Mohs surgery wounds will require stitches or other techniques to help them close and heal properly.
How Long is Mohs surgery?
Mohs surgery can take between half a day to the entire day. The actual Mohs surgery itself only takes several minutes and the reconstruction of the surgical wound can take 30 minutes. Most of the time is spent waiting for processing and analysis of the tissue specimen.
Who Should Have Mohs Surgery?
Mohs surgery is appropriate for many individuals with nonmelanoma skin cancers, such as basal cell carcinoma and squamous cell carcinoma. The level of precision associated with Mohs surgery maximizes the preservation of healthy tissue, making it especially appealing for the treatment of skin cancers in functionally and cosmetically sensitive locations, such as the face, scalp, neck, hands, and shins, and feet. In other less cosmetically and functionally sensitive areas of the body, it can be used to treat skin cancers that are larger, have previously been treated but recurred, do not have clearly defined edges, or display aggressive features under the microscope. Official Appropriate Use Criteria have been developed that help determine which skin cancers are most appropriate for treatment with Mohs surgery.
How Is Mohs Surgery Performed?
Mohs surgery typically involves five steps:
1. Anesthesia
Mohs surgery is performed using local anesthesia, which involves less risk than general anesthesia. At the beginning of the procedure, the area of interest is cleaned, then numbed with a mixture of lidocaine and epinephrine. While there may be some slight stinging or burning associated with the injection itself, the area around the injection quickly numbs, making the rest of the surgery painless.
2. Tissue Removal
The skin cancer is first debulked, allowing the physician to explore how deep the cancer penetrates beneath the skin. A thin layer of the surrounding tissue is then removed and a dressing is applied over the wound.
3. Tissue Mapping and Examination
The layer of tissue that was removed is then labeled, mapped, processed, and mounted on a slide. All of this is done at an on-site laboratory. Creating a finished slide with the tissue specimen is the most time consuming part of the Mohs surgery day, taking between 1-2 hours for each stage. The slides are then examined under the microscope by the Mohs surgeon at the on-site laboratory, and the results are interpreted. Areas where skin cancer still remains is mapped accordingly.
4. Additional Tissue Removal
If the first layer displays residual skin cancer, another small layer of skin is removed from the cancerous areas only. This sample is again labeled, mapped, processed, and mounted on a slide for examination under the microscope. This process is repeated until all tissue removed is found to be cancer-free, at which point the excisional wound is prepared for closure.
5. Reconstruction
With the all of the cancer removed, the wound is then closed. The science of wound closure is complex and involves a profound knowledge of tissue anatomy and movement, balanced by knowledge of aesthetic outcomes. Based on the size and location of the wound, closure may involve simple side-to-side closures, flaps, or grafts. Sometimes, the wound is left open to heal by itself.
Preparing for Mohs Surgery in NYC
Medications
Certain medications can increase the risk of excess bleeding during the surgery. To reduce this risk, avoid taking ibuprofen, vitamin E, ginkgo, ginseng, and fish oil during the two weeks prior to the procedure.
Blood thinners such as aspirin, Plavix and Coumadin can also increase bleeding during surgery, but should continue to be taken if prescribed due to a previous serious condition such as a stroke, heart attack or blood clot. Discuss this with your Mohs surgeon during your surgical consultation.
On the day of your consultation, be sure to bring a list of all current medications, including vitamins and herbal supplements. Because the surgery can last several hours, any medicine needed during the day should be brought along as well.
Smoking
Smoking can affect the healing process for wounds. Avoid smoking for two weeks before, and two weeks following Mohs surgery.
The Day of Surgery
On the day of surgery, eat normal meals such as breakfast before arriving. Because the procedure may take between half a day to the entire day, consider bringing your lunch. Many patients also bring books or other entertainment to help pass the time while their tissue is being processed.
Recovering After Mohs Surgery
Initial Recovery
Before leaving, the physician will schedule a follow-up visit in one to two weeks to remove any stitches and evaluate healing.
While most wounds from Mohs surgery aren’t particularly painful, bruising and swelling may appear following the procedure and can last for up to two weeks. If pain relief is needed, acetaminophen (Tylenol) is recommended over ibuprofen or aspirin.
Skin Checks
It is important to continue regular skin cancer screenings following any diagnosis/treatment of skin cancer. These should be conducted every three to six months.
Scarring
While Mohs surgery generally yields better cosmetic outcomes than its other surgical alternatives, scarring is an expected outcome of the procedure. Depending on the location and extent of the cancer, secondary cosmetic dermatology procedures such as laser or surgical scar revision may be recommended to help improve its cosmetic appearance. Note that the appearance of the scar will continue to spontaneously improve for up to a full year following the procedure.
Schedule a Mohs Surgery Consultation in NYC Today
Choosing Wall Street Dermatology for your Mohs surgery means choosing unmatched expertise, personalized care, and exceptional outcomes. Led by Dr. Julia Tzu—a triple board-certified dermatologist and one of the few in NYC with dual fellowship training in both Mohs surgery and dermatopathology—our practice offers a level of precision and cosmetic finesse that few others can match.
Don’t settle for less than the highest standard of care—book your Mohs surgery consultation with Dr. Tzu at Wall Street Dermatology today.